When care and support planning for a service user, there is a structure to the approach nursing and care staff should use which will ensure the care plan is fit for purpose. It does not matter if the care plan is on paper or a digital care planning system, the same rules apply. Some people know it as the care planning process, while others might know it as the nursing process. Either way the stages involved are:
Assessment requires the person undertaking the care and support planning to involve the service user, the people important to them and often other health and social care professionals. Involving the service user and others enables the care and support planning assessment to be more holistic and person-centred, https://www.cqc.org.uk/guidance-providers/regulations-enforcement/regulation-9-person-centred-care.
What Holistic Means
What Person-Centred Means
In care the assessment process requires all of the skills of the assessor to get it right, this includes good communication with the service user and their family. Such information gathering involves collecting subjective data, that is data which is about how the person thinks and feels and which is unique to the individual and can only be gathered by asking them.
Some of the process is objective, or at least semi-objective, and might include tools such as MUST and Waterlow designed to help care staff understand people’s care needs in a meaningful and structured way. Objective data might also include things like the service user’s medical diagnoses, date of birth etc.
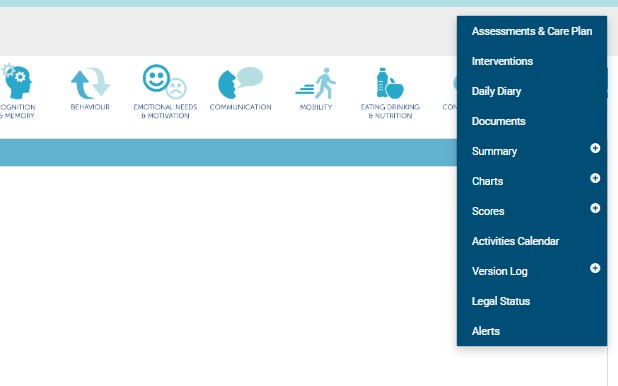
Either way tools such as the care and support planning app from careis, https://www.careis.net/features/, enables the person undertaking the care and supporting planning assessment to do in a structured way.
The app enables care staff to proceed though a series of questions about the individual and their needs, wants and wishes covering all of the activities of daily living. This ensures that the assessment process is complete, holistic and that nothing is overlooked as the care staff start to formulate, with the service user a plan of care.
enables care staff to proceed though a series of questions about the individual and their needs, wants and wishes covering all of the activities of daily living. This ensures that the assessment process is complete, holistic and that nothing is overlooked as the care staff start to formulate, with the service user a plan of care.
Plans of care and all that goes after them are only as good as the original assessment. This means care and nursing staff should take the time to get this part of the process right. It is fundamentally important that the assessment process is used to get to know the service user in as much detail as possible because failing to do so may lead to a failure in care, neglect or, at worst, abuse.
In order to demonstrate good care to the CQC and other regulators, care staff should be able to show how they started their assessment processes prior to admitting the person to the service. Such pre-admission assessments and care and support planning enable the service to understand the person’s care needs and identify if they, the service, are able to meet them. Failure to undertake a pre-admission assessment properly can lead to an early breakdown in the relationship between the service user and the service, mean that the service cannot meet the person’s needs and ultimately to placement failure.
 As with all assessments therefore, pre-admission assessments and care and support planning must be person-centred and holistic if they are to be meaningful; this is one of the reasons they should be undertaken by an experienced, trained and competent staff member.
As with all assessments therefore, pre-admission assessments and care and support planning must be person-centred and holistic if they are to be meaningful; this is one of the reasons they should be undertaken by an experienced, trained and competent staff member.
In later blogs in this series, we will discuss other aspects of the care and support planning process, like the planning, implementation and evaluation of care and how care staff and nurses can get these right first time.
Careis are currently giving away a copy of Patient Assessment and Care Planning in Nursing by our CEO Peter Ellis when you sign up for our Care and Support Planning App. In the book there is more detail about the issues discussed in this blog and much more regarding assessment and care planning.